Sadly, you’re not looking at a baby belly… this is a tumor-filled belly 😩 The last couple of months have been incredibly challenging. Just as I was starting to feel a little stronger a few weeks after surgery in August, other symptoms began to show up or worsen, and have only gotten more difficult to cope with since then.
I had scans in early October which showed continued progression. I haven’t been able to do much for integrative treatments in several months now because my body screams a hard NO!! whenever I try. I do push, because I want this stuff to work, I want to heal, but there has been no clear payoff with anything lately.
I have literally begged and pleaded with surgeons and other doctors to help me: specifically with a very large liver mass. Every single consult and plea has been met with a closed door, and sadly, little to no compassion. I had begged the surgeon in August to do everything he possibly could while he had me opened up, but he said he would only take the largest mass, and then we would discuss further interventions after I’d had some time to recover. However, when that time came, I received a hard No to any further care from him. I’ve consulted with multiple specialities and surgeons across different health care systems. None will help me. They see me as too high risk and a lost cause without much time left.
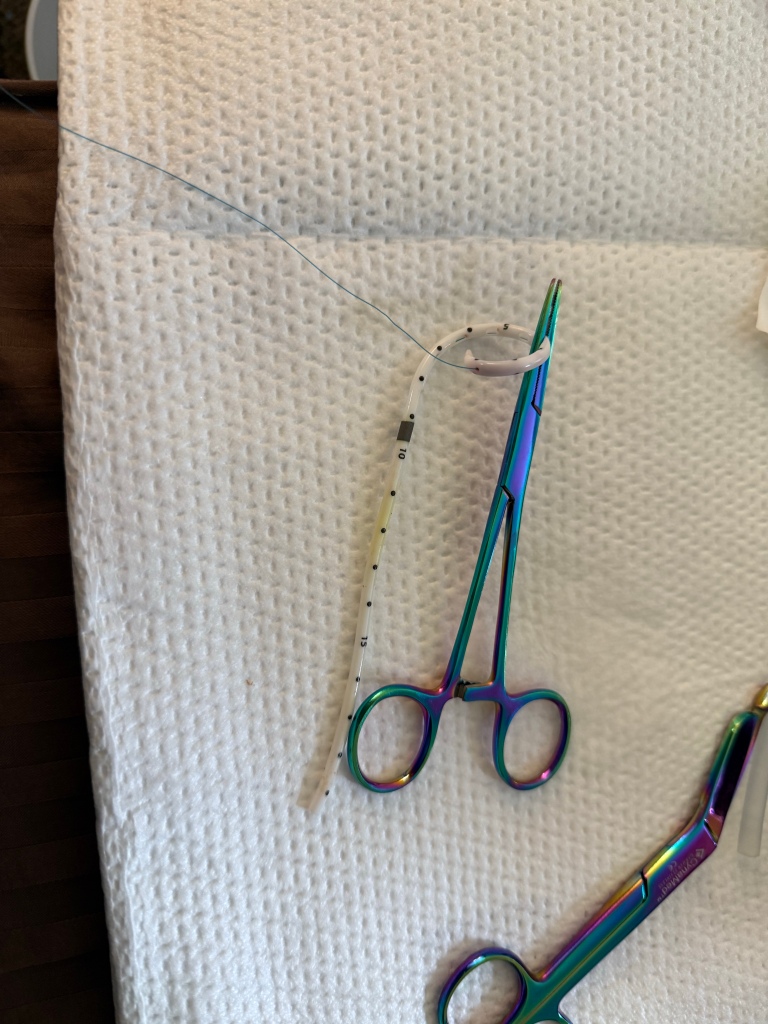
The only conventional provider I can find who is willing to try anything on the large liver mass is my radiation oncologist. I am set to start proton beam radiation this coming week, and the treatment course is expected to take about a month. I have no idea what to expect, but because of the large size and location, as well as involvement of the inferior vena cava, the rad onc is worried about how sick I could get. Idk how much I’ll be able to eat, keep down, detox, or digest… I already have terrible abdominal pain and pressure, and because of the restricted blood flow in the IVC, I get extremely short of breath, weak, with heavy, painful, shaky legs any time I bend at the waist or take even 2 stairs. Lymph and blood flow are restricted below the liver, so I have a lot of fluid retention, lymphedema, and more nerve pain now. Many mornings are spent on the couch writhing in pain for hours as I try to deal with the severe radiating pain down my leg, in my low back, and through my whole abdomen. Sadly, nothing really works to alleviate the pain.
What’s probably one of the hardest things to deal with is knowing I have a bunch of integrative tools at my disposal, but my body simply won’t tolerate them anymore. When I push, I’m met with horrible reactions that last days and only result in further tumor swelling/growth.
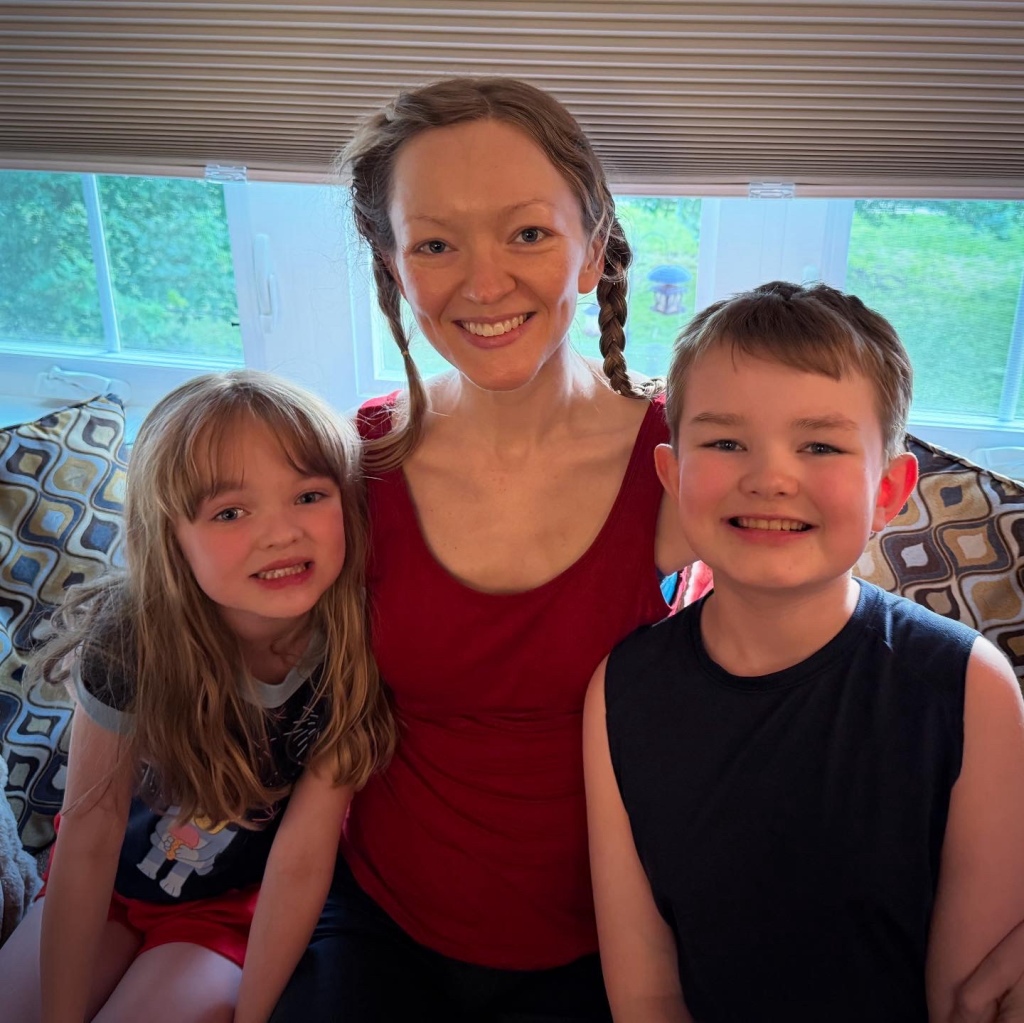
Needless to say, I have been very lost and simply incapable of doing much more than trying my damnedest to survive each day. Life barely feels real anymore.
I have SO many negative emotions toward certain providers and their lies, misinformation, inflammatory statements, and omission of extremely critical information over the last 6 years. I am working to process all of this, because I know it isn’t doing me any good. As both a patient and provider though, it makes me completely disgusted with the way conventional oncology is run in our country. There have been some angels in this hell, but unfortunately it isn’t the norm.
Six years in, and there are very few stones I’ve left unturned. Yet here I am, fighting for my life harder than I ever have, with seemingly few options remaining. I still believe, somehow, someway, there IS a path to true healing for me. I don’t know what it is. My senses don’t perceive it. But my heart and soul believe.
I don’t know what the next month will bring with treatment, or if I’ll have the capacity to keep everyone updated. Honestly, right now, I can Barely take care of my Very basic needs each day. Thank you in advance for your understanding, prayers, and support.